Spinal Tuberculosis
Spinal Tuberculosis
Spondylolisthesis
Slipped Disc
Spinal Stenosis
Sciatica
Cervical Spondylosis
Vertebral Compression Fractures
Scoliosis
Kyphosis
Myelopathy
Osteoarthritis
Spinal Infections
Spinal Cancers
Spinal Cord Injury (SCI)
Cauda Equina Syndrome
Ankylosing Spondylitis (AS)
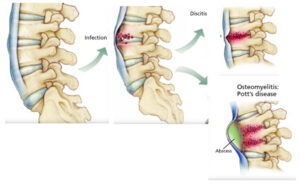
Spinal Tuberculosis
Spinal tuberculosis is a serious and debilitating condition marked by a gradual process of bone destruction, which can ultimately result in the collapse of vertebrae. This destructive process may involve multiple vertebrae and lead to a swift breakdown of the bone structure, ultimately resulting in a kyphotic deformity.
As the disease progresses, the kyphotic deformity can exert severe compression and stretching forces on the spinal cord. This compression can have grave consequences, potentially leading to paralysis of the lower limbs. Given the potentially devastating impact of spinal tuberculosis, early diagnosis and timely medical intervention are essential to prevent further deterioration and mitigate the risk of paralysis.
Spondylolisthesis
Spondylolisthesis is a condition characterized by the displacement of one of the vertebral bones in your spine, causing it to slip out of its normal position and rest on the vertebra below. This condition is a significant contributor to lower back pain, particularly because it frequently occurs in the lower back region.
While spondylolisthesis is more commonly associated with the elderly population, it can also affect younger individuals who engage in sports like football, gymnastics, and weightlifting. Some experts suggest that genetics may be a contributing factor in determining certain individuals’ susceptibility to this condition.
Treatment for spondylolisthesis typically involves a comprehensive approach, which may include physical therapy, pain management, and, in severe cases, surgical intervention. It is important to consult with a spine surgeon for an accurate diagnosis and tailored treatment plan based on individual needs.
Slipped Disc
A slipped disc, often referred to as disc prolapse or disc herniation, does not involve the actual slippage of the disc itself. Instead, it occurs when the inner, softer portion of the disc known as the nucleus pulposus bulges outward due to a weakness in the outer part of the disc. This bulging disc may exert pressure on the nerve roots originating from the spinal cord. In addition to compression, inflammation can develop around the prolapsed portion of the disc, irritating the nerve root and causing swelling, which further intensifies pressure on the nerve.
It’s worth noting that disc prolapse can manifest in any part of the spine, but it is most commonly observed in the lower back, specifically in the lumbar spine, followed by the neck or cervical region, and rarely in the thoracic spine. Within the lumbar region, the levels most frequently affected are L4-L5 and L5-S1. The size of the disc prolapse can vary, with larger prolapses typically leading to more severe symptoms.
Treatment options for disc prolapse may encompass a range of approaches, including conservative management with rest, physical therapy, and pain relief medications. In cases where conservative methods prove insufficient, surgical intervention may be considered, such as microdiscectomy or spinal fusion, depending on the severity of the condition and the patient’s specific needs.
Spinal Stenosis
The spinal cord serves as the conduit through which nerves travel from the brain to various parts of the body. When the space surrounding the spinal cord narrows, it can result in the compression of adjacent bones, potentially causing damage to the nerves. This condition is frequently encountered in the lower back and neck regions.
Individuals often remain unaware of this issue until they begin to manifest symptoms, which can include pain, tingling sensations, numbness, muscular weakness, and various other discomforts. Recognizing these symptoms and seeking prompt medical evaluation is crucial for addressing spinal cord compression and preventing further complications.
Treatment options for spinal stenosis vary depending on the severity and underlying causes. Conservative approaches may include physical therapy, pain management, and lifestyle modifications. In more severe cases or when conservative methods prove ineffective, surgical intervention may be considered to relieve pressure on the spinal cord and nerves, thus addressing the issue and preventing further complications. It’s essential to consult with a spinal surgeon to determine the most appropriate treatment plan based on individual needs.
Sciatica
Sciatica is characterized by pain stemming from the compression or irritation of the sciatic nerve, one of the longest nerves in the body, originating in the lower back and extending down to the lower leg. The onset of sciatica pain is frequently associated with factors such as a herniated disk, bone spur, or other spinal conditions that affect the nerve. This sharp and often intense pain radiates from the lower back, traverses deep into the buttock, and extends down the lower leg. It’s important to note that sciatica pain is typically experienced on one side of the body.
Effective treatment for sciatica typically involves a combination of approaches tailored to the individual’s specific condition. Conservative measures such as rest, physical therapy, and pain relief medications are commonly employed. For cases resistant to conservative treatments or those involving severe symptoms, surgical interventions like discectomy or laminectomy may be considered to alleviate nerve compression and provide relief from sciatica pain. Consulting with a spinal surgeon is essential for a precise diagnosis and the development of a personalized treatment plan.
Cervical Spondylosis
Cervical spondylosis is a common condition that arises due to the natural degeneration of spinal discs in the neck as you age. This degeneration causes the discs to gradually dry out and shrink, resulting in conditions such as osteoarthritis, disc herniation, and the development of bone spurs. It’s worth noting that approximately 90 percent of individuals affected by this issue are aged 60 or older, and these changes are typically considered a part of the natural aging process. However, it’s important to acknowledge that symptoms may only manifest in a minority of cases.
Management of cervical spondylosis typically involves a range of conservative measures tailored to the individual’s specific symptoms and needs. These may include physical therapy, pain management, and lifestyle modifications. In cases where conservative approaches prove inadequate or when severe symptoms are present, surgical interventions like cervical fusion or discectomy may be considered to address the condition more effectively.
Vertebral Compression Fractures
Vertebral compression fractures are common occurrences, often associated with the natural aging process. These fractures typically result from the weakening and compression of the spinal vertebrae, leading to a reduction in vertebral height. They are frequently caused by conditions like osteoporosis or trauma.
Osteoporosis, a common condition in older adults, can weaken the bones and make them susceptible to fractures, including vertebral compression fractures. Trauma, such as a fall or accident, can also cause these fractures in individuals of various age groups.
Treatment for vertebral compression fractures aims to alleviate pain and improve spinal stability. Conservative approaches, including rest, pain management, and bracing, are often the initial strategies. In some cases, minimally invasive procedures like vertebroplasty or kyphoplasty may be recommended to stabilize the fractured vertebrae.
It is important to note that vertebral compression fractures can be associated with varying degrees of pain and discomfort, and individualized treatment plans should be discussed with a spine surgeon for optimal management.
Scoliosis
Scoliosis is characterized by an atypical sideways curvature of the spine, a condition frequently detected in adolescents during the rapid growth phase just before puberty. While the primary cause of scoliosis is often unknown, it is commonly referred to as idiopathic scoliosis. One noticeable sign of scoliosis is uneven shoulders in affected individuals. In some cases, scoliosis may arise due to congenital defects in the spine, a condition known as congenital scoliosis. It can also be observed in patients with conditions like cerebral palsy and neuromuscular dystrophy.
Treatment for scoliosis depends on the severity of the curvature and its impact on an individual’s health. In mild cases, regular monitoring may be sufficient. For more pronounced curves or if scoliosis is causing pain or other complications, treatments may include bracing or surgical interventions to correct the spinal curvature and restore alignment.
Kyphosis
Kyphosis is a condition characterized by an excessive forward bending of the spine, often referred to as a “round back” or, in severe cases, a “hunchback” deformity. This condition is most commonly observed in elderly patients, particularly those with multiple osteoporotic compression fractures of the spine. However, kyphotic deformity can also result from spinal tuberculosis or traumatic injuries. Additionally, it may occur due to congenital defects in the spine, known as congenital kyphosis.
In severe instances, this deformity can exert pressure on the spinal cord, potentially leading to paralysis and the loss of control over bowel and bladder functions. It is essential for individuals with kyphosis to seek medical evaluation and treatment, as appropriate, to manage the condition and mitigate potential complications.
Myelopathy
Myelopathy is a condition characterized by impaired functioning of the spinal cord and nerve roots, often resulting from compression. Several factors can contribute to the development of myelopathy, including trauma, arthritis, bone spurs, degenerative disc disease, or disc herniation. It is most commonly observed in the cervical and thoracic regions of the spine. Individuals experiencing myelopathy may encounter difficulties with manual tasks, reduced dexterity, and challenges performing activities as simple as buttoning shirts. Additionally, they may exhibit gait instability and balance issues while walking.
In more severe cases of myelopathy, patients can become bedridden, with a loss of bowel and bladder control. Given the potentially debilitating nature of this condition, prompt medical evaluation and appropriate treatment are crucial for preventing further deterioration and enhancing quality of life.
Osteoarthritis
Osteoarthritis, a condition characterized by the degeneration of cartilage at the ends of vertebrae, can result in significant pain and stiffness within the spine. This protective cartilage, found in the neck and lower back discs, serves to prevent friction between the vertebrae. However, as it wears down over time, it can lead to the development of spinal osteoarthritis.
Osteoarthritis tends to affect women more frequently than men and often worsens with the passage of time. Individuals grappling with this condition may experience substantial discomfort and a decrease in their spinal mobility. Timely medical evaluation and appropriate management are crucial for alleviating symptoms and improving the quality of life for those affected by spinal osteoarthritis.
Spinal Infections
Spinal infections encompass a spectrum of conditions that can lead to back pain and neurological issues. Alongside tuberculosis, bacterial (pyogenic) and fungal infections of the spine can give rise to these problems, collectively referred to as spondylitis and spondylodiscitis.
These infections are typically characterized by the invasion of pathogens into the spinal tissues, often leading to localized pain, fever, and, in severe cases, neurological deficits. Spinal infections can develop through various means, including hematogenous spread from other body regions, direct contamination following surgery or trauma, or extension from nearby structures.
Early detection and timely intervention are critical in effectively managing spinal infections. Treatment strategies may involve a combination of antibiotics or antifungal medications, surgical drainage of abscesses, and, when necessary, spinal stabilization procedures to address structural damage.
Spinal Cancers
The spine is susceptible to skeletal metastasis, a condition where cancers originating from various organs, including the breast, prostate, lung, and kidney, spread to the spine. This metastatic spread can result in symptoms such as severe pain, spinal cord compression, and even paralysis. Individuals with a history of cancer in other parts of the body or those who have undergone cancer treatment and experience back pain should undergo a thorough evaluation.
In addition to metastatic tumors, primary spinal tumors can also affect patients. These tumors may include osteoid osteoma, osteoblastoma, giant cell tumor, aneurysmal bone cyst, and aggressive hemangiomas. Furthermore, tumors can originate directly from the spinal cord itself, comprising types like meningioma, schwannoma, and neurofibroma. Additionally, the spine may be impacted by blood plasma cell disorders such as multiple myeloma.
Early detection and appropriate management of spinal cancers are crucial to effectively address the condition and alleviate associated symptoms.
Spinal Cord Injury (SCI)
A spinal cord injury (SCI) is a life-altering event that transpires when the spinal column experiences sudden, traumatic impact, resulting in damage to one or more vertebrae, ligaments, or discs. This damage can lead to a loss of essential functions, including mobility and sensory perception. Traumatic spinal cord injuries can occur due to various incidents such as vehicle accidents, sports-related injuries, falls, gunshot wounds, knife wounds, and similar events that inflict trauma upon the spinal cord.
In addition to traumatic causes, nontraumatic spinal cord injuries can also occur, stemming from conditions such as arthritis, tumors, infections, or disc herniation in the spine. These nontraumatic injuries may gradually manifest and lead to debilitating consequences for individuals.
The management of spinal cord injuries necessitates a multidisciplinary approach, encompassing medical interventions, physical therapy, rehabilitation, and assistive technologies, all tailored to the specific needs of the patient. Early intervention and ongoing care play a crucial role in optimizing the recovery and quality of life for individuals impacted by spinal cord injuries.
Cauda Equina Syndrome
Cauda equina syndrome is an exceptionally rare yet critical condition involving the spinal nerves. The cauda equina, a bundle of nerves stemming from the lower back region of the spine, plays a pivotal role in facilitating communication between the brain and various organs in the pelvis, as well as controlling the function of the legs. This intricate network of nerves can be adversely affected by conditions such as a herniated disk, spinal fracture, or any other pathology that compresses this nerve bundle.
Cauda equina syndrome represents a surgical emergency, demanding immediate surgical intervention to avert potentially enduring consequences, including leg paralysis. When left untreated, this condition can lead to profound neurological deficits, emphasizing the urgency of timely diagnosis and prompt surgical management.
Ankylosing Spondylitis (AS)
Ankylosing spondylitis (AS) is a relatively uncommon yet impactful chronic arthritis type, affecting a limited portion of the population. This inflammatory condition can lead to the fusion of the small bones within the spine and rib cage, resulting in a rigid and inflexible spine. In such stiff spines, even minor falls can lead to fractures, which can pose significant challenges in terms of management.
Over time, AS contributes to discomfort and stiffness in the spine, gradually diminishing its flexibility and ultimately resulting in a stooped posture. This condition is not limited to the spine alone; it can also affect other joints and organs within the body. AS exhibits a predilection for young males, being more prevalent in this demographic than in females, and may involve a genetic component.
In severe cases, AS can lead to severe kyphosis and a loss of the ability to maintain an upright gaze, further underscoring the importance of timely diagnosis and appropriate management to preserve spinal function and overall quality of life for affected individuals.